17 mm Anterior Inferior Cerebellar Artery (AICA) Aneurysm Treated Endovascularly by Flow Diverter 10/13/22
My Story
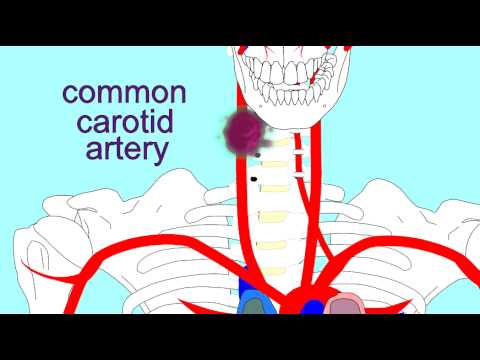
I was diagnosed on 9/9/22 with a 17 mm aneurysm in my left Anterior Inferior Cerebellar Artery. 30 years ago, this might have been a death sentence. 15 years ago, it would have required a craniotomy. However, it was treated on 10/12/22 endovascularly using a FRED device (flow diverter). I wanted to share my story for anyone else undergoing a similar experience.
I will be 62 in November. I am 5’ 9”. I have been fairly active all my life, with no comorbidities. I was only slightly overweight from sitting on the couch during the pandemic.
Diagnosis
In April, 2022, at the end of a bout of long Covid, I developed a ringing (tinnitus) in my left ear. I thought it was an ear infection. Thinking it would resolve itself, I delayed going to a doctor and in June went hiking in the Adirondack Mountains in NY, and also in late August hiked to 8,000 feet on Mount Rainier in Seattle. In August I saw two different ENT’s. The second ENT ordered an MRI which I finally had on Friday 9/9/22.
9/10/22: News of Aneurysm
On Saturday 9/10/22 I got an urgent call from the ENT that my MRI revealed a very large, 15 mm, aneurysm in my left Anterior Inferior Cerebellar artery, and that I should go straight to the emergency room because I was in imminent danger of a stroke.
I spent Saturday afternoon and early evening getting a CT scan in the ER. The CT showed the same thing as the MRI.
Besides the ringing, I had no other symptoms. So they told me to come back for an angiogram procedure next week which I did.
The angiogram showed that my aneurysm was even bigger than the CT indicated. Now up to 17+ mm. The outer edges of my saccular aneurysm were clotted over.
9/11/ -10/12: Gathering information, Angiogram Results, Second Opinions
Unlike some others on the forum, my aneurysm was so large that everyone thought it should be operated on right away. There was no real option to “wait and see.” Technically, would call my aneurysm “saccular” and “fusiform.” But to me it looked like a giant testicle, or an octopus’ floppy head. It was not just a “swelling” or bulge in an artery, it was like another organ growing in my skull. Even I, with one glance at my angiogram, thought I needed to get something like that out of my head.
Additionally, my neurosurgeon could flip through the angiogram images like a motion picture showing us very weak blood flow through the sac. It didn’t seem to me that there could be great blood flow to the distal end of the artery.
One Month of Anxiety, Anxiety, Anxiety
I am lucky to live in Seattle. It happens to have a world-renown endovascular surgeon. Probably several of them. However, in my surgeon’s and my initial discussion of the MRI and CT he started off with “Why don’t we just block off that artery?” And we had a discussion about what loss of brain function in the cerebellum would mean!! (Argghhh!)
I had done some research at this point, so I asked him, “Couldn’t we put a flow diverter in there?”
He suspected that the artery was too narrow to be able to insert a flow. However, he said the angiogram might give us more information.
After the angiogram, my neurosurgeon came to my bedside and said that in addition to the aneurysm, the artery was a little swollen, so he thought he could, after all, get a flow diverter in there.
To this day, I am still not sure why he led off with the “why not just cut off the blood flow?” question. Maybe it was a Socratic technique and he was going to circle back to the other options to show how good they were.
Second Opinions & Patient Education
In any case, the mere thought of having voluntarily choose blocking and artery and losing brain function, left me very nervous. 3 weeks ago I had been hiking at 8,000 feet on Mount Rainer! Happy the pandemic was over. Never heard of an aneurysm! Never heard of clipping, flow diverters, stents, meshes. I had never had any surgery or been in the hospital except to visit others. I had heard of craniotomies, a friend of mine had two of them; the recovery process from my friends subdural hematomas was really terrifying.
I also felt that I was living on borrowed time. The fear of the 17 mm aneurysm bursting was intense. It put a lot of pressure on my decision making.
Researching the Internet was informative. It gave me a lot of the language and history around aneurysms.
However, I want to include here some words of caution about Internet research. I am not saying don’t do it. But you must take what you find with a grain of salt. Here are some tips around this:
First, if you are like me, anxiety high, you will be desperately craving more information and discussion about aneurysms. Personally, I do think there needs to be a way to have more discussion. AND I think it is very hard to get this discussion, particularly if you must make a decision quickly.
I think there are two types of discussion needed:
- Technical or intellectual discussion. Wanting to understand which is the best procedure.
- Emotional discussion. – As patients, we want to know we are not going to die on the table, or come out like Jack Nicholson. If you’ve never had surgery before, basic fear is a big issue. There is a part of us that is just afraid of the unknown.
A tip I could offer about dealing with anxiety is that surgeons are great at part a) above, but not so good at part b), emotional reassurance.
What helped emotional reassure me was talking to my surgeon’s head nurse; Physician assistants and interns didn’t help that much, but an experienced nurse did. They see these issues all day and they are looking at patient outcomes, not the technical details. They are trained to deal with patient anxieties and this is a really, really valuable skill. As a patient, the surgeon will be great at telling you all about edge cases and surgical failures, but they don’t seem to understand that sometimes there is a part of us that does not want to hear about the 1% chance of failure. As patients, it’s not that we want 100% risk-free surgery. We know there are risks. We just want to know that we are basically going to come out OK. It’s a feeling-thing, not an intellectual thing.
The nurse not only told me that it was normal to have anxiety, but also things about endovascular procedures no one else told me such as:
- If the artery started to clog up, they can use different blood thinner meds to prevent it from happening.
- They do ultrasounds on the blood flow speed in your brain to detect if things are flowing and they can also detect “micro clots” before any really bad clots happen.
- They can go back in again with a catheter which can inflate your artery with a balloon, just like they now do for heart arteries.
- There is a follow up 1 month after your surgery.
- There is another angiogram 6 months after surgery.
In other words, even though endovascular procedures can get you out of the hospital sooner (only one night in the hospital!), they don’t just send you home and wait and see if you stroke out. They have some ways of monitoring and intervening if something goes wrong. This knowledge calmed me down a lot and was something I could not find on the Internet.
Another thing that helped me (I did not find this out till the day of the procedure), is that the flow diverter starts to work right away. In other words, in the pictures on the Internet, flow diverters seem to have very wide meshes. It seems like the blood could flow right through them. I was worried that even after surgery I would still be at risk for the aneurysm bursting. But my surgeon informed me that risk goes down immediately after placing the flow diverter. I think this is a little bit in contrast with coiling.
Again, I think I was lucky to live in Seattle and to live so close to the neurosurgical hospital (less than 6 miles). If I lived in a distant city, I probably would make plans to stay close to the hospital for a few weeks after the surgery. If surgery goes well, you can cancel the hotel plans, but in the meantime you are close to the experts who know what they are doing and who can, in fact, monitor you. (see below for more about this.)
If I had to have the procedure done in distant city, I would make plans to stay in that city for about 1.5 weeks after getting out of the hospital.
A Little More Info on Second Opinions
There are online organizations and hospitals online which offer second opinions for aneurysms for a very low price. In my situation, these looked to be a reasonable way of being a good consumer. The real attraction was getting more discussion. It was not that I did not trust my surgeon; it was just all a lot to absorb in a month’s time. I really needed a “medical therapist.”
I signed up and paid money with three of these places. They all said they would get back to me in two weeks.
Two of the online second opinion places which I paid money to never got back to me at all, and the third got back to me in three weeks, which was then after my surgery, and the only thing they said was they needed more imaging. These were disappointing results. It was really the local neurosurgical nurses that helped me in the end (see above).
If you have a small aneurysm and you are in a “wait and see” mode, getting second opinions makes some sense. This was not my situation. I could hear the tinnitus in my ear changing tones and my aneurysm was huge. I was not in a “wait and see” mode. I needed information quickly.
Perhaps the inexpensive online places – perhaps their heart is in the right place. I think there should be a place where people can discuss their anxieties and get some info on the latest techniques. But the bottom line is that a) these places are going to request all your imaging, not just an iPhone photo of your angiogram, and b), you are probably going to need to travel to the 2nd opinion location in person.
It seems to me there is still a “hole” here for people looking for basic discussion about aneurysms. Your local nurse organizations might be the place for that.
It is very, very difficult to know if you are doing the right thing. In the end, all you can do is a little Internet research and look up the reputation of your surgeon. People told me that you want to find the surgeon who has done this 100 times before. In my case, I was lucky that I had such a surgeon, and despite my anxieties, I trusted him. It was a weird combination of trust and anxiety. In searching for second opinions, I ended up phoning places where my surgeon had worked before and everyone, everyone spoke of him very highly. That helped too.
Endovascular vs. Open (Clipping) Procedures
Internet research will tend to show you
a) a good deal of useful information, mixed with
b) outdated articles, and
c) some “medical propaganda.”
As I see things, there is still today (2022), a war going on between the endovascular approaches vs. open surgeries (craniotomies and such) .
It must be difficult for traditional surgeons to adjust to the endovascular approach: classical surgeons train for decades to be able to open people up and cut out bad parts. But now, along come these “surgeons” who actually don’t cut much of anything, they just push little tubes though people’s arteries up into their brains. Not only is this completely different than traditional surgery, these new endovascular guys are taking surgical business! They are making the classical surgical approach obsolete.
On the Internet, you will find scholarly articles for both sides. You will encounter advocates of the clipping approach who claim the blood thinners used for the endovascular approach are dangerous. You can also certainly find endovascular experts who point to the risks or opening the skull.
You can get lost in these different scholarly articles.
To me, NOT opening my skull seemed like the best approach, but I was worried about future complications with endovascular procedures, such as bleeding from my aneurysm the first time I took a blood thinner, and clotting 5 years from now. I had nightmares about a titanium-nickel tube in my head causing an infection or something.
IMHO, there is not enough information for the lay public on the new endovascular approaches, and the field is changing rapidly. 5 years ago it was all about coiling, but things are rapidly moving in the flow diverter direction. 5 years from now it will change again.
In the end, I asked both my general practitioner and also the ENT who first discovered the aneurysm (I just begged him for 5 minutes of his time), about which was the safer procedure. (My ENT was also a well-respected surgeon). Who, after all, was I to know? I’m a software engineer. I could do three more months of research and I still wouldn’t know. It wouldn’t turn me into an expert.
Both my GP and the ENT said that “if something could be treated endovascularly, it was generally the better way to do it”
I had also seen a friend’s craniotomy and had been with her when she came out from surgery. She required serious care for a month afterward. This certainly inclined me towards endovascular.
In addition, the hospital here in Seattle was into the endovascular approach.
So, still with a lot of anxiety, I got in an uber at 6 am and headed to the hospital. It was still dark when I arrived at the hospital and I could see the stars.
I wondered if that might be the last time I would see them.
That kind of gives you my mental state. I didn’t have all the answers, but just enough to feel like I was doing the right thing.
Flow Diverters vs. Coiling
- A respected health professional told me that people who had coiling tended to be in the hospital a lot longer, while they made sure the coiling seats properly.
- From an engineering standpoint this makes sense to me, and it helped me think I made the right decision.
Surgery Facts not to Worry About
Things to know if you have never had surgery before:
- There will NOT be a lot of waiting around. Even if you’re scheduled for early in the morning. These guys do this for a living 5 days a week. My hospital staff was a well-oiled machine.
- You don’t need to bring things to read or computers. don’t bring them because the pre-op room is small. You won’t have time.
Facts about All Procedures Including Angiograms
- When you arrive at the hospital and go to the pre-op room, the first thing they do is take all your clothes and give you an a paper thin hospital gown.
- This will likely leave you very chilled.
- In addition, as they wheel you down to the operating room, there is a breeze in that air-conditioned air which will further chill you. The cold is to keep the germs dow.
- You should ask for warm blankets and try to put them over your feet, so the breeze on the way to the operating room doesn’t go up under your feet.
- Do everything you can to conserve your body heat.
- The #1 thing I remember about my angiogram was the chill, especially on the way to the operating room.
- So the 2nd trip, for my actual aneurysm procedure, I ordered a BESKAR Rechargeable Hand Warmer from Amazon, turned it on as I changed into the gown, and kept it under the small of my back until they came to get me for the actual procedure. I think it helped a lot.
Modesty
- Forget it about it.
- After they get your gown on, they’re going to shave your privates.
- You’ll have like 5 people around you, attractive nurses, etc. and they will just lift up the front of your dressing gown.
- They need to do this in case they can’t get a catheter up your wrist, they use your femoral artery. I guess hair is bad for wounds, so you’re going to get a Brazilian, regardless if you are a man or woman.
- If you’re a woman, they probably will give you male nurses because that’s the way the universe works.
Suggested Hydration Protocol
- People in this forum recommend drinking a lot of water to keep your blood vessels hydrated, making it easier for the nurses to find them for IV’s, arterial lines, and catheters. This makes some sense.
- However, if you are anxious before the procedure, you might have to pee a lot. That happened to me during the angiogram. 5 or 6 times after undressing I had to go pee. I had to pee 1 before going into the operating room!
- When you need to pee, you have to walk though the hall with your ass exposed. A minor point.
- Therefore, for my aneurysm procedure, I drank a lot of water during the week (I ordered a crate of bottled water), but then stopped the late afternoon before my procedure.
What’s In the Operating Room
- Chills: It’s very cold on the way down and in the operating room, until they put you on the table, which has the “airbags” inflated with warm air. The airbags are heaven.
- Pain?: In my hospital, I never felt anything when they inserted the catheter or when they inserted the arterial line. They must have very good local anesthetic.
- I was “awake” for my angiogram, but for my aneurysm procedure they gave oxygen first, then told me “you will feel a burning in your left arm,” which was the anesthesia going in.
- I read in this forum about the tough as nails woman who remained awake during her procedure. But I had no interest in being awake and I think my neurosurgeon would not have allowed it.
- So I was out before I could say “Oh, yeah, I feel the coldness in my arm.”
- Once you are out they will insert a “foley” in your penis or urethra, but you will be out so you don’t know it.
- And you will be intubated, but you won’t know that either.
- The above was for my aneurysm procedure. For my angiogram (imaging), I did not have a “foley,” I was not intubated, and I was only partially anesthetized.
- I admire the above woman who had her procedure without going under, but have no regrets about going fully under. If anyone has a wire in my head and I’m not supposed to move, just knock me out and strap me down.
- My procedure ended up being 2.5 hours.
- I understand that the surgeon went in twice with two different flow diverter types. This was because I had a very weird right angle bend in my artery that he was not sure he could negotiate around.
Post-op in Hospital: What to Expect
- There is generally a post-op room right outside the operating room. You will likely wake up here, before going to intensive care.
- There’s a good chance you will throw up after general anesthesia. This will likely happen when you get up to intensive care and they have a saline IV in you. Don’t worry about throwing up. It came and went quickly, at least for me.
- You will have a sore throat from being intubated. You can drink hot water, but eating a little bit of a grilled cheese sandwich is what cleared the sore throat for me. Don’t worry about the sore throat either.
- I did spend just one night in the hospital. Surgery was 8 am to 11:40. Then they wheel you to intensive care, where you might puke, wrestle with your throat, drink water, etc.
- After a few hours you start to feel better. Nurses come in an out and eventually ask you if you would like something to eat.
- I was very dizzy for 4 hours after the procedure. When I moved my head to say yes or no, it made me a little nauseous. That faded by the morning.
- The kitchen will probably close at 7 pm, so it’s good to order something.
- You will probably have a headache to some degree, so they keep the lights low in intensive care. You wake up a lot. Night nurses come in and visit you.
- 5 am the day after the procedure they took out my arterial line. This is not fun. The nurse will have to put a lot of pressure on your wrist because you are on blood thinners. They are supposed to hold the pressure for 20 minutes.
Post-Op Breathing Procedures
- Your lungs might hurt after anesthesia, especially when taking a deep breath.
- There are some procedures for clearing the anesthesia out of your lungs and for waking up. Here is a procedure that even a week after surgery I could feel helped me (https://www.uhs.nhs.uk/Media/UHS-website-2019/Patientinformation/Respiratory/Tips-on-a-speedier-recovery-after-surgery-patient-information.pdf )
- I highly recommend these breathing procedures.
10/15-10/22 Post Procedure Complications/Events/Headaches
- I did feel ready to leave the hospital after only 1 night.
- I did not have much of a headache.
- I actually walked out of intensive care (no wheel chair) down to my sister’s car. So I felt ready to leave.
- However, that night at my sister’s house I woke up with a bad headache and a strong throbbing in my left ear where the mild tinnitus had been. When I sat up in bed, the headache was much better. I thought the headache was partly due to anesthesia, partly due to laying down on my side, which I had not done in intensive care. In the morning the headache seemed more like a “tension” headache and I could massage most of it away.
- However, the second night I had a very similar headache, but more focused in the left side of my head where the bad artery was.
- The second night headache could not be massaged away, and I could not lay down to sleep. I tried to sleep sitting up, but I wasn’t able to.
- So I decided to go back to the hospital and get checked out. I didn’t think I was having a stroke, because I didn’t see any face drooping or other signs. But something was not right, I felt.
- The hospital did another CT scan which showed no problems. They called my surgeon and he prescribed the steroid Methylprednisolone which was like a miracle cure for that night. No pain. Good sleep.
- Methylprednisolone is a steroid. It makes you hungry for meat. Get a nice steak.
- The next day my surgeon called and said the pain was probably from the aneurysm shrinking quickly. That might not have been the full cause; I think after stretching an artery or two is going to require some readjustment.
- I finished my last pill of Methylprednisolone today. I have had some strong headaches the week I was on them.
Bottom Line: I did have some headaches after this procedure. Today, 9 days after the procedure, was almost headache free. I was also tired and needed naps.
I recommend taking the week off from work, or a little longer. Take two weeks or three weeks. If you return early it’s easier than asking for more time.