Dear all,
I hope you are well ![]()
My Annie exploded 5 years ago and got coiled. Now my neurosurgeon prospects a second operation to put a flow diverter. He said it’s a more delicate operation but then I should be without worries for 20-30 years (well…I’m 53, let’s see ;-)). Be also said that the convalescence will take one year … And that not everyone reacts well to the blood thinners one has to take from two months before operation until… (until one year or maybe for all my life).
I trust my neurosurgeon 100% but I am of course scared of another operation and of “what can go wrong” and also of this uncertainty regarding convalescence and blood thinners etc.
And I have to decide if I do the operation now or if we wait and see.
Anyone with experience on this who wants to share?
Big thank you!
Iris
I had a rupture early this year & Coiling was done same day and flow diverter was put in about 4 weeks later. In my case the aneurysm neck was wide at 6mm and flow diverter was put in place to keep the coil stable. I am on blood thinners but not sure how long I will have to keep taking them. How wide is your Annie neck?
Hello @iris
Its good to hear that you are doing well five years down the road from the rupture. I have a similar history, but the difference is that I was recommended to do a second procedure six months after the rupture. My aneurysm had a wide neck and due to the shape and location of the aneurysm, it couldn’t be fully treated with coils when it ruptured. My neurosurgeon recommended a stent and more coils to fully treat the aneurysm. I learned that I had to be on a dual platelet medication for six months and then on Aspirin for the rest of my life . I expressed my concern about this situation due to a few other medical problems and I was told that I could have the option to watch and wait , but the aneurysm had to be taken care of in the future. The neurosurgeon looked me in the eyes and told me that there is a slight chance of a new rupture in the future, and if it happens, I wouldn’t survive and it was better to take care of this sooner rather than later.
It was like being between a rock and a hard place…….
It took me a week or two to process the information and to make a decision, I searched for information on our site, I read research articles, I consulted my primary care physician, talked a lot about it with my family and I took many long walks…… I came to the conclusion that it was necessary to get it done, I couldn’t live with the knowledge that it might rupture again. The stent and coils procedure was made 14 months ago and everything went well, the recovery was a mild breeze compared to the initial rupture. I was on a dual anti platelet medication for about six months and now I’m on Aspirin 325mg daily and that will hopefully change to a baby Aspirin when I have my next checkup in the fall.
Did I easily bruise ? Yes.
Any complications with bleeding elsewhere? No.
Any GI discomfort? No, I was also prescribed Pantoprazole as a protection for the stomach lining when I was on a higher dose of Aspirin.
This is my story and to sum it up, so far, so good. I’m glad we took care of it and I’m almost back to my old self.
I understand that this is a standard procedure for the condition we have and we have many members that can pitch in.
Good luck ![]()
Good Morning @iris and everyone else! I had a stent placed on my 4th procedure as the neck wouldn’t close off. So about 7 years for me. My Neurosurgeon had said I’d be on it for about six months then down to 325 aspirin and then hopefully work down to 81 mg aspirin. I was on Plavix for a month or two prior and down to 325 mg Aspirin for a very short time and now the 81 mg Aspirin for the rest of my life. I have other health issues as well, fragile skin being the one I guess the anti platelets didn’t get along with and any bump was difficult to stop bleeding. A bandaid (plaster) can do a lot of damage to me but I learned to use a powder, or gauze and Vet wrap (can’t remember the name for humans, @oct20 might know it…)
My Neurosurgeon took me off the stronger ones rather quickly as compared to others here. The day she put in the stent was the first time we heard my Neurosurgeon say that she was confident she had it closed off. I just had to wait long enough for medical science to develop a stent that could be used in the location of my aneurysm.
Recovery seemed quick to me, much quicker than from the rupture. It felt like overnight but in reality was probably several months. My neuro issues aren’t gone, but they have diminished an incredible amount since my stent was put in. I met the new NP at Neurology and he didn’t know I had all my issues as they didn’t present the day we met! I had one major setback when we went to a friend’s wedding that took a few months to recover, the NP at Neurology was so concerned he ordered an MRI/A and wanted me to have my Neurosurgeon look over them. No concerns from my Neurosurgeon and I can honestly say the stent she used has been extremely helpful. One of the things I can do now is actually say a number correctly i.e. 2:35 used to be two three five as I’d stutter on the 30 but now I can say two thirty five without stopping. A small thing for some, a huge thing for me!
Dear @Rizwan6532 @oct20 @Moltroub and all,
First of all, thank you so much for sharing your experience. My neck was only 1 mm (“was” at my last check Oct 2021) but the aneurysm is slowly growing (still, a small one, 4-5 mm). My Neurosurgeon said also that we could wait and see but that placing a flow diverter would finally close the aneurysm and avoid a second rupture and having to make a second operation in an acute situation again.
It took me 4 months to decide and I finally signed up for the operation. The waiting time here (Austria) is pretty long due to lack of personnel and as I am not an urgent case I will probably do the operation sometime next year. I have concerns about it but the idea of having to face again a rupture in some years time when I will be more “aged” is not reassuring, therefore I have decided to go for it. My situation is similar to yours @oct20 and yes, it seems like a standard procedure for what we all have. Something that until 10 years ago they were not doing but now it’s the perfect solution for unclosed annies.
I’ll also have to be on dual platelet for 6 months and then Aspirin for… ? no idea - maybe the rest of my life, hoping that all will go well!
Thank you all for reassuring me and let’s hope for the best! Good luck to us all ![]()
Iris
Good for you Iris! To take control of what we can is a huge step for ourselves and you made a giant leap IMHO! Unfortunately a shortage of medical personnel is worldwide I assume. My last procedure was also considered elective so on hold I went and then the follow up angiogram I didn’t know anyone on her team. For me that was unsettling as many had been there through all my angiograms and knew which music I liked and joked around with me. If I may ask, does your doctor plan on doing another imaging in six months or so, just to see how your aneurysm is doing?
@Moltroub Thanks! I guess I’ll have to do another imaging before the operation, I should do one anyway in October for my annual check - no idea if the standard check after operation is also every 6-12 months, but I’ll keep you posted. And yes, Covid had a huge negative impact on medical personnel everywhere in the world.
Now that I took the decision and signed up for the operation, I am feeling better, relieved. What scares me (but I try not to think about it) is the 5% possibility of something going wrong in the operation (these are the statistics) and that there is no way to know it in advance… but I think with all what we already went through, this is normal. ![]()
By the way: Very happy to read about your improvements after operation! Thanks for sharing ![]()
![]()
![]()
Thanks so much Iris! I’m uncertain to the risks statistics you’re referring to, cna you share the study, please ma’am? I just read an article on nih that was quite interesting, though didn’t have the risks stats. The authors were quoting some very old statistics though all the way back to 1961! Surely there’s more recent numbers with the improved technology is what I thought. I don’t discount the risks of everything from anesthesia on, it’s why I have a litany the morning of a procedure with my Neurosurgeon…did you sleep well last night, did you eat breakfast, did you go potty, how’s your allergies doing? One of her new team members years ago became quite miffed with me and said she’s a neurosurgeon. I said in my stutter, she’s human first and I certainly don’t want her sneezing, doing the potty dance, not fully awake or her brain wanting to know why she didn’t eat whilst guiding a catheter up my body in a main artery. A couple more angiograms later and he let me know he fed her as I had to wait until late afternoon for mine. She had some emergencies to deal with and they all know I don’t mind waiting. I’ve always imagined someone was pushed out of their slot so she could save my life!
Iris I am sorry to hear that this course of treatment is so different to that which I experienced and which I hear about more commonly in US. My Aneurysm
was in a precarious location and it was determined that the only viable solution was a flow diverter. I was on a blood thinner for several months, then graduated to a full strength aspirin and now take a baby strength aspirin for the rest of my life. A small price to pay for the result. I am told that the Aneurysm has stopped growing, so the flow diverter is doing its job.
It is surprising to me that your procedure is considered elective considering the amount that your Aneurysm has grown since your clipping. I wish you the best.
Dear @BrianS @Moltroub and all,
Thanks for sharing! And here are some more info to recap the situation: in Oct. 2017 I had an aneurysm rupture that was immediately coiled. My recovery was pretty fast I would say (when it happened, my left eye was paralysed and closes. It stayed so for two months, then started slowly to open up but still with double vision and then slowly it started to move normally and my vision was normal again).
From that moment on, I had to do 6 months checks, then once a year checks and now I have been offered the flow diverter operation - elective because the neck is open only for one millimetre and I’ve been told it is not so risky.
To all who are on medications after the flow-diverter operation: do you find that your life has changed for the better and what are the limitations you have?
@Moltroub the statistics I was referring to are quoted from the talk with my neurosurgeon, who said that 95% of the cases goes well and 5% have complications. In the “everything goes well” scenario flow diverter is described as the perfect solution because once done there are nothing to worry about for 20-30 years. So, until I’m 73-83 I should live worry-free ![]()
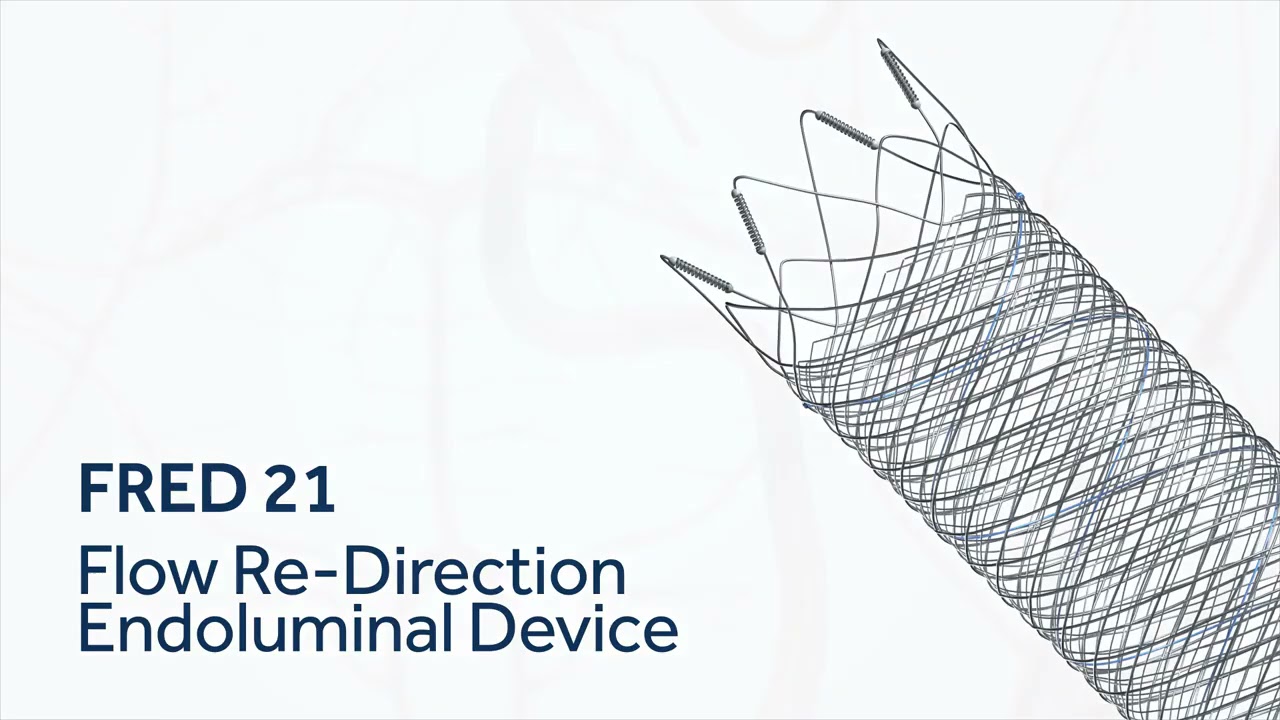
I’ve done my homework and found some videos online, in case someone is interested:
I’ve been told that until 10 years ago there was no other way than “wait and see” after a coiling) and that once the flow diverter is in place, the aneurysm will naturally shrink and close.
The 5% risk is the “usual risk” of an operation with full anaesthetics, plus what can go wrong in this kind of cases… that is still not 100% clear. He mentioned that some people don’t react well to the medication pre and post operation and then I read the full list of risks (you know, that list that they give you to sign for the authorisation…) and well, not a funny reading at all…
My main concern is very human and I can sum it up to: “I was already so lucky to survive to an aneurysm rupture and now, after 5 years, I am healthy: why should I go through another operation? Do I really risk to have another rupture?” But then I thought that hopefully all goes well and that it is always better to have a planned operation instead of waiting for something serious to happen and then having to react in an acute situation.
Here in Vienna the hospital is among the best in Europe for neurosurgery and I fully trust my neurosurgeon and his stuff, but I’m sure they would do different choices if they had more personnel. Let’s see…
All the best to you all and keep on smiling ![]()
Thank you for your support!!!
Ciao!
Iris
@trust_level_0 Oh my gosh Iris! Thank you so much for, well everything! Thank you especially for clarifying the 5%! It helped me to understand.
And yes ma’am, the long list of things that can go awry is mind boggling, not on my fun list either. If I recall correctly, the majority is with anesthesia. When I had my stent put in I had a wonderful RNA that promised he would do his best to put and keep me in my happy place😂. He did and when I woke up, I woke up rather quickly and was doing really well. It was the first procedure that didn’t set me back for months.
I know we have a lot of members who have had a flow diversion stent put in, I’m hoping they’ll come and tell their experience. I’ve done a broadcast (hopefully) to all our members. I don’t often do it so I may have gotten it wrong.
To install my stent, I was on generic Plavix prior to my procedure and then 325 mg aspirin afterwards and quickly put on just 81mg aspirin which I will take the rest of my life apparently. The aspirin is enteric coated aspirin which helps coat the stomach, etc from any potential damage as I understand it.
Hi y’all - I’m not sure I can help but I will share my experience. When I had my subarachnoid hemorrhage in January, 2018, I also had an unruptured one on the other side (posterior communicating artery). They coiled both. However, the medication they sent me home with to prevent vasospasms literally made me sick as a dog.
They ended up stenting one side in April, 2018 as angiogram showed problems. Angiogram in August of 2018 was okay. Plavix then 325mg then 81 mg aspirin
They switched to MRAs I guess in 2019 or so. MRA in 2021 was abnormal and they stented the other side (through the wrist this time) was placed on Brillinta in conjunction with 81 mg aspirin. Followup MRA in August of 2021 showed tiny residual of most recent stent. Neurosurgeon hoped that when I was off the blood thinner it would close off the rest of the way. Brillinta stopped in October of last year.
I guess I find out later this month whether he was right about it sealing off but he told me last October that I “have an awful lot of hardware” in my head. My first thought was well no chit, you put it there but I didn’t say it.
The surgical nurse did tell me when I went back for my second angiogram and I told her about my stabbing head pains that most people that had the stents suffered from those. Something my doc never told me because he pronounced me fixed. lol
I’m still taking 81 mg aspirin.
And I’m very sorry, I forgot my manners, I wish you luck with your procedure!!!
I can add my experience here. I got coiled 20 years ago after an accident. From that i was suffering frequent headaches and ocular migraines that got worse over the years. 3 years ago there was found another aneurysm in that area, 7mm wide necked probably because of a weakened vessel due to the accident decades ago. The doctors said flow diverter would be the best choice. So i had it done and had a quick recovery without major issues since 2019. Sometimes headaches, but far and in-between and not too bad. Migraines are gone too. I take plavix 75mm daily with no issues because i can’t stomach the aspirin. Last mra from spring shows everything is still fine. So i am glad I had that done. The benefits outweigh the risks IMO. Chances are everything will be ok. All the best to you all! If you have any questions feel free to text me.
Sincerely
Stefan
I there! I was diagnosed with a giant aneurysm of 35mm in October 2018 (unruptured), got clipped and a flow diverter two weeks later. I took clopidogrel for 6 month in combination with aspirin, now only 100mg aspirin per day for the rest of my life. I´m fine so far, but the annie is still there and there is still a little blood flowing through it (maybe because it was so big). I noticed the annie because of double vision, still experience a blurred vision from time to time, but not so often. Headaches occur, mostly in the evenings, but they are acceptable.
All in all the procedure was ok, and the recovery too. At the moment I have some strange neurological issues with tingling legs and arms, but doctors aren´t sure if that has to do with the annie.
I wish you luck - everything will go well!
Ferret
2 posts were split to a new topic: Pain after ruptured aneurysm
Hi Iris-Can I ask what your surgeon meant by ‘there is nothing to worry about for 20-30 years’? I had my flow diverter placed 10 years ago at the age of 34 and that’s a bit worrisome! Thank you!
Hi Restolz! Sorry - I did not mean to scary you… I’m not sure if he meant (since I’m 53) that I would be ok until the end of my days or, literally, 20-30 years. I will ask him next time I see him (which could be in several months) and will get back to you. But if your neurosurgeon did not say anything like this, then don’t worry at all. ![]() …I know, it’s not easy…
…I know, it’s not easy… ![]()
All my best to you and all and thank you again everybody for sharing your own experience! Very useful!
Ciao :-* Iris
Thank you for the quick response! Please do let me know if you find out anything else. Hope you’re doing well ![]()
If you Trust your neurosurgeon then do exactly as he suggests. I am on a 325 aspirin for the rest of my life and people I am around understand the consequences of my bumps and how I bruise easily.
As for your concerns and another operation, your surgeon has your best interest at heart (and his reputation).
Forget About the What Ifs and Focus on the Positives!! (My Mantra)
Hiya,
I’m not sure if what I can add will be sufficient, since I am so new to all this, but I have to go back and have an angiogram in 6 months (8 months after my coiling and stent).
See what an angiogram will say, then listen to your dr. they really know best. I know it’s scary, but they are the experts. If you have a good relationship, and they have a good reputation, then you have to trust them.
My .02 cents.
Best of luck to you… xo
~Julie